Answer to Mid-Month Mindbender
Cytophagic histiocytic panniculitis, HLH (Hemophagocytic lymphohistiocytic) syndrome
Let’s look at the puzzle in a different manner
Bumps skin deep (skin nodules) ; high spikes it stings (high spikes of fever)
Good store (ferritin) in ‘press’ (iron); Wow! it’s ‘stress’ (increased ferritin level is as acute phase reactant)
In our world though, not always ‘bad’ as you call (not malignant always just to differentiate it from SPTCL)
Gobbles up whole (cytophagocytosis) , spits blood in the mix (extravasation of RBCs and hemosiderin in histopathology)
Low in ‘numbers’ (reduced blood counts of RBCs, Leukocytes or platelets), troubles yet to fix.
The photograph showed engulfed intact RBC, neutrophils inside macrophages, suggestive of hemophagocytosis.
Multicentric reticulohistiocytosis (MRCH)
First photograph shows ‘ground glass’; it indicates the cytoplasm of the giant cells seen in MRCH.
Second photograph shows histiocytic collection in the dermis with giant cells.
Third photograph shows the X Ray of the hands with characteristic bilaterally symmetrical erosive arthritis and deformity of the finger joints.
TRAP is Tartarate resistant acid phosphatase, an iso-enzyme of the group of acid phosphatases, which is highly expressed by activated osteoclasts and macrophages. It usually stains positively in histiocytic infiltrate of MRCH.
Secondary syphilis
The first two pictures are to remind us about the ‘Tuskegee Syphilis Study’ which was widely discussed due to unethical recruitment and execution of the study. The histopathological photomicrograph though of low power still shows the reaction pattern of secondary syphilis with a dermal infiltrate characteristic of lichenoid pattern at the top and a significant deeper perivascular infiltrate which is discrete. The higher power shows the composition of infiltrate with predominance of plasma cells.
The leaf on the other hand has typical ‘moth-eaten appearance’, a characteristic of syphilitic alopecia seen in secondary syphilis patients.
Secondary syphilis is a better answer than syphilis as the histopathological features of the other two stages (primary and tertiary) don't show a reaction pattern like this.
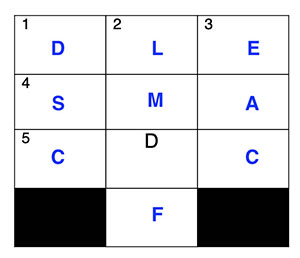
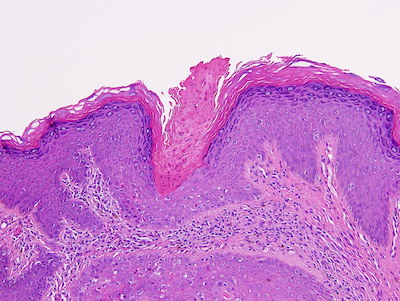
Inflammatory linear verrucous epidermal nevus (ILVEN)
ILVEN presents as linear intensely pruritic hyperkeratotic erythematous papules that coalesce to form plaques along the lines of Blaschko, usually in the first few years of life.
Microscopic findings: There are sharply demarcated alternating zones of orthohyperkeratosis and parakeratosis in a horizontal direction overlying psoriasiform hyperplasia of the epidermis. The granular layer is absent beneath the parakeratotic zones and thickened beneath the orthokeratotic zones of hyperkeratosis. The rete ridges are elongated and thickened. Mild spongiosis is also present. Upper dermis shows moderate perivascular lymphocytic infiltrate.
Differential diagnosis includes linear psoriasis which shows confluent parakeratosis and thinned rete ridges.
Dermatofibroma
Dermatofibroma is a better answer than lipidized dermatofibroma.
Dermatofibroma usually presents clinically as a hyperpigmented firm nodule (I’m darker than the rest). In histopathology the epidermal changes are acanthosis, increased basal layer pigmentation that is localized just above the dermal tumor. The tumor is usually located in upper mid dermis with a Grenz zone that can be narrow to wide (Little distant from the top) and the tumor lies horizontally giving a lenticular shaped architecture. There are numerous histopathological subtypes that have been described. The lipidized variant in particular is frequently seen around the ankle and shows foamy histiocytes as one of the infiltrates (Bit ‘fatty’ over the ankle).
The composition of the cells in the tumor is usually a mixture of spindled fibroblasts, histiocytes sometimes with lymphocytes, giant cells (Kind of ‘mixed’ of the lot). Rather in the case of DFSP the tumor is more monomorphic with spindled fibroblasts (boring).
Traversing chords and fascicles of spindle cells are usually seen inside the tumor as typical arrangements. The storiform pattern is seen in dermatofibroma but less pronounced than that of DFSP (My distant cousin, Always has a better 'stori' to tell).
Sunlight/(ultraviolet + visible light)
The right half of the picture shows clinical lesion of porphyria with pauci-inflammatory sub epidermal blister and the test tube containing centrifuged urine sample of patient showing red fluorescence.
The right upper histopathology picture showed solar elastosis in the form of bluish fibrillar structure in the upper dermis.
The right lower picture indicates UV signature mutation of C→T at a di-pyrimidine site.
So, all the sequence of events are related to sun exposure.
Leishmaniasis
The first picture is that of a ‘chiclero’, a collector of ‘chicle’ from trees for production from chicle gum in Latin America and Mexico. They used to suffer from cutaneous leishmaniasis of the ears also known as ‘Chiclero ulcer’
The second pic is related to the discovery of the species. Both have connections to India. William Bong Leishman, an army medical officer who performed an autopsy of a spleen specimen from an English soldier posted in Bengal and discovered the protozoan parasites using microscopy in 1900. In 1903 British medical officer Charles Donovan, who was serving in the Indian Medical Service, had found the parasites at the Government General Hospital in Madras.
The third pic depicts a marquee sign. The arrangement of intracellular amastigotes in tissue specimens sometimes mimics that of a signboard commonly being used in earlier days.
The last pic is showing the area which are endemic for visceral as well as primary cutaneous leishmaniasis in India and around. The eastern part of the country is endemic to visceral disease caused by L. donovani,whereas the areas of Kashmir valley, Bikaner in Rajasthan and Satluj river valley in Himachal are endemic to primary cutaneous leishmaniasis by predominantly L. tropica, rarely L. major and donovani (in Himachal).
Langerhans cell histiocytosis
The first line indicates its similarity in clinical presentation with seborrheic dermatitis. Though it has few other features including solid papules, plaques overall scaly plaques over the scalp can mimic seborrheic dermatitis. As infantile seborrheic dermatitis tends to improve with age, persistent seborrheic dermatitis-like lesions in a child who has completed infancy should alert the clinician to give Langerhans cell histiocytosis (LCH) a thought: an old school teaching. The so-called ‘geographic skull’ appearance in imaging is a feature we see in aggressive systemic variant of LCH. ‘Court’ and ‘Ace’ are the word related to lawn tennis. These were a clue to indicate the viewers about ‘Tennis racket’ shaped organelles i.e Birbeck Granules inside Langerhans cells.
The photomicrograph shows a predominantly lichenoid tissue reaction with moderately dense upper dermal infiltrate, which is the predominant pattern we see in LCH.
Keratosis lichenoides chronica or Nekam’s Disease
The first image indicates the ‘linear’ and ‘reticulate’ pattern of skin lesions.
Second image showed erythema and crusted plaques over cheeks and nose. It is a common cutaneous presentation of the disease in question.
The third image is a low power histopathological picture showing significant epidermal changes with hyperkeratosis, irregular acanthosis and parakeratosis along with a band like upper dermal infiltrate.
The fourth image of higher magnification showed few necrotic keratinocytes at the dermo epidermal junction. The histological feature is that of a lichenoid tissue reaction with significant epidermal hyperplasia.
Nekam’s disease or keratosis lichenoides chronica is characterised by rough, scaly plaques over extremities and trunk. The plaques characteristically have a linear or reticulate pattern. It runs a chronic course and has facial involvement characterised by rosacea or seborrheic dermatitis like lesions.
The common link between the pictures is Parakeratosis.
Pic 1: Showing a focal spongiotic tissue reaction with parakeratosis of the stratum corneum.
Pic 2: The related movie (PK) indicates the short form of parakeratosis.
Pic 3, 4 and 5 indicates skin lesions with diagnostic parakeratosis-related features in histopathology.
The parakeratosis pattern of the three disorders are illustrated below:
Pic 3 is that of porokeratosis; the biopsy from the thready margin shows cornoid lamella which is a parakeratotic column in the epidermis with underlying additional epidermal and dermal findings.
Pic 4 is of pityriasis rubra pilaris which shows checkerboard pattern of (vertically and horizontally alternate) parakeratosis.
Pic 5 is that of axillary granular parakeratosis identified histologically through the typical pattern of parakeratosis as the name suggests. There is actually retention of the keratohyalin granules in the stratum corneum which is also thicker than normal.
Non bullous neutrophilic lupus erythematosus
We particularly wanted the identification of the skin lesions in the answer.
The clinical photograph provided showed erythematous plaques over face and histopathology showed a predominantly dermal neutrophilic infiltrate, atrophic epidermis and focal vacuolar interface changes. These are somehow a strange combination to explain.
The clue in the text indicates SLE with some skin lesions which have plenty of neutrophils. The last line indicates a lesion which is non-bullous. Neutrophils are not common in skin histopathology of lupus erythematosus. Bullous LE shows neutrophils in the form of papillary tip microabscesses like dermatitis herpetiformis. Nonbullous neutrophilic lupus is a recently described entity. It usually presents as erythematous plaques or nodules over extremities, trunk, face without much constitutional symptoms. The lesions are well responsive to systemic corticosteroids. Histopathology usually shows mild atrophic epidermis and upper and mid dermal interstitial and perivascular infiltrate of predominantly neutrophils. The infiltrate may extend up to the subcutis. The reaction pattern in dermis mimics that of sweet's syndrome. A notable difference might be the significant proportion of cases showing interface dermatitis additionally and DIF positivity at the basement membrane.
(Brinster NK, Nunley J, Pariser R, Horvath B. Nonbullous neutrophilic lupus erythematosus: a newly recognized variant of cutaneous lupus erythematosus. J Am Acad Dermatol. 2012 Jan;66(1):92-7)
Sporotrichosis caused by the fungus Sporothrix schenckii
The first two lines indicate an ‘asteroid’ (it is believed that an asteroid impact at the end of the Cretaceous period led to a mass extinction of the dinosaurs), a clue towards 'asteroid body', which we see in histopathology of various disorders under the microscope. The third line indicates the nonspecific nature of the finding in histopathology. Asteroid bodies are the products of unusual microtubule dynamics in monocyte-derived giant cells. (Gadde PS, Moscovic EA. Asteroid bodies: products of unusual microtubule dynamics in monocyte-derived giant cells. An immunohistochemical study. Histol Histopathol. 1994 Oct;9(4):633-42.). It has been demonstrated in various disorders including sarcoidosis, sporotrichosis and other deep fungal infections, foreign body giant cell reactions, necrobiosis lipoidica etc. The classical clinical presentation of sporotrichosis has been described as lympho-cutaneous disease with nodules and ulcers arranged in a linear distribution along the lymphatics. The organism is found in the environment in decaying vegetable matter, hays etc. In the early nineties widespread incidence of sporotrichosis was described at various parts of the world in sphagnum moss handlers.
(Coles FB, Schuchat A, Hibbs JR, Kondracki SF, Salkin IF, Dixon DM, Chang HG, Duncan RA, Hurd NJ, Morse DL. A multistate outbreak of sporotrichosis associated with sphagnum moss. Am J Epidemiol. 1992 Aug 15;136(4):475-87.)
Lupus vulgaris
First pic is of Niels Ryberg Finsen, a physician and scientist from Faroe Island, who used the concentrated light radiation treatment for various diseases notably lupus vulgaris; and later, was awarded Nobel prize in ‘Physiology and Medicine’ 1903.
Second pic denotes face and buttocks as common sites affected by Lupus vulgaris. In Europe face is the commonest site, but in India buttock including lower limb are commoner sites involved.
Third pic, denotes a tuberculoid granuloma, a reaction pattern commonly found in histopathology of lupus vulgaris.
Fourth pic is that of a wolf; (in latin: lupus). In initial description the clinical lesions of lupus vulgaris was described as 'ravages of wolf' for having disfiguring and destructive lesions over face. (Interesting to note that in Europe wolf is the most dangerous predator, they don’t have lions and tigers so wolf bite probably was considered most disfiguring)
1 All the pictures show: artifacts or processing artifacts
Figure 1: Folding artifact
Figure 2: Pseudolipomatosis: due to improper fixation
Figure 3: A mounting artifact due to a trapped air bubble. Air bubbles are formed under the cover-slip when the mounting medium is too thin and as it dries, more air gets sucked under the edges.
Figure 4: Autolytic changes: an artifact due to delayed fixation
Figure 5: Decalcification artifact
2 Figure 2 and 4 indicate fixation artifacts while others occur either before or after fixation.
Clue 1
Beautiful are they, in whom I stay,: indicates towards 'Lepra Bonita' or 'Beautiful leprosy' the other name for Lucio leprosy.
Far from you, by the Pacific it may;: It is endemic in Mexico, a North American country at the pacific coast.
Vessel it is, sometime I creep: During Lucio reaction there is usually infiltration of lepra bacilli in to the endothelial cells of the small and medium size vessels.
Symptoms are less than what it seems: The reaction is differentiated from necrotic ENL by lack of constitutional symptoms
You have to 'fight' to pick me right.: 'Fight' sounds like 'Fite', the stain used to demonstrate the organism in tissue specimen.
Clue 2
The picture showed classical retiform purpura like lesions seen in Lucio phenomenon. It happens due to vascular occlusion by infiltrating lepra bacilli inside endothelial cells.
A Chronic granulomatous disease (CGD)
B Nitroblue tetrazolium dye reduction test (NBT) and Dihydrorhodamine (DHR) assay by flowcytometry
The biopsy shows presence of multiple epithelioid cell granulomas in the dermis. There is mild lymphoplasmacytic infiltrate in the perivascular location. No necrosis is identified.
Features are of a granulomatous cheilitis.
Granulomatous cheilitis can be seen in a wide spectrum of diseases. It can be idiopathic, or may be associated with a systemic disorder, such as sarcoidosis or Crohn’s disease. At times, it can be the first manifestation of the underlying systemic disease.
In the given case, the child had a history of recurrent infections (recurrent ear discharge, lower respiratory tract infection, soft tissue abscesses). It appears to be a case of primary immunodeficiency disorder (PID). PID shows a wide clinical spectrum, which is increasingly recognised currently. There are many varieties of PID, which can be diagnosed with combined immunological and genetic testing.
The given child showed homozygous defects in NCF1 (c.73_74del GT, frameshift, p. Tyr26HisfsX25). This is a hallmark genetic alteration (in addition to others) in chronic granulomatous disease (CGD). CGD is an inherited primary immunodeficiency disorder, with a defect in neutrophilic phagocytosis. Both infective and non-infective granulomas involving the visceral structures as well as skin are characteristic of this entity.
The history, histology and genetic analysis in this case is diagnostic of CGD with orofacial granulomatosis/ granulomatous cheilitis. It is a rare, but important condition associated with granulomatous cheilitis.
The other immunological tests that can be done to confirm the diagnosis are:
Nitroblue tetrazolium dye reduction test (NBT): no dye reduction is seen.
Dihydrorhodamine (DHR) assay by flowcytometry: showed reduced NADPH oxidase activity.
Among these, DHR is more sensitive and specific for CGD and done in most advanced laboratories.
These indicate a defect in neutrophilic phagocytic activity. Both these tests were positive in this child.
Serum immunoglobulin level and lymphocytic population are usually normal.
There are defects involving five genes. A genetic testing is useful for confirmation of the diagnosis as well as helpful for family screening.
A This is a BIOCHIP mosaic, used for diagnosis of autoimmune bullous diseases
B The principle of its use is indirect immunofluorescence (IIF).
Biochip mosaic is a commercially available device, which is used for diagnosis of various autoimmune blistering diseases (AIBD).
There are different kits available, with different number of wells. The wells are covered with antigens, which can be derived from primate mucosa, cultured cells, transfected cells or protein extracts. Patient serum with adequate dilution is added to the well, and then FITC coated anti-human IgG is added. If there is presence of antibody against a specific antigen, it will give a positive result in the respective well. This is mostly used for subepidermal AIBD.
Merkel cell
Synaptophysin, chromogranin, CD56, CK20
We can see a cell with a lobulated nucleus and presence of neurosecretory granules/ dense core granules in the cytoplasm. The nucleoli are small. There are no tonofilaments, desmosomes, hemidesmosomes, menalosomes or Birbeck granules.
This is a neuroendocrine cell, consistent with the Merkel cell. They are present in the epidermis. These cells give rise to the Merkel cell carcinoma, a high-grade neuroendocrine carcinoma of the skin.
They can be stained with synaptophysin, chromogranin, CD56, CK20 (dot-like positivity).
a. Martius Scarlet blue and phosphotungsctic acid hematoxylin
b. Fibrinogen positivity
The histology picture shows multiple veins in the dermis and subcutaneous tissue are distended and show presence of thrombus in their lumen. There is no evidence of vasculitis. The accompanying arteries do not show any thrombosis. There are many conditions which can produce preferential venous thrombosis, including superficial venous thrombosis, protein C or protein S deficiency, paroxysmal nocturnal hemoglobinuria, cryoglobulinemia and many others.
To confirm the fibrinous nature of the material, special histochemical stains should be performed, which include Martius Scarlet blue (MSB) and phosphotungstic acid hematoxylin (PTAH). MSB is a trichrome stain that is very sensitive for fibrin. It stains fresh fibrin as red and organized, old fibrin as blue.
Direct immunofluorescence (DIF) is usually negative for immunoglobulins (heavy and light chains) and complement. Thrombi show positivity for fibrin on DIF. However, if it shows immunoglobulin heavy chain positivity or light chain restriction on DIF, a possibility of myeloma associated thrombosis should be suspected.
a. There is loss of INI-1 expression.
b. Myoepithelial carcinoma (cutaneous)
The histology picture shows a malignant tumor in the dermis composed of epithelioid to polygonal cells. These cells have moderate amount of cytoplasm, and show frequent mitotic activity.
The common differential diagnoses include metastatic carcinoma, sarcomas with epithelioid morphology (epithelioid sarcoma, epithelioid malignant peripheral nerve sheath tumor, epithelioid angiosarcoma, epithelioid leiomyosarcoma, etc), myoepithelial carcinoma, malignant melanoma (although there was no junctional activity or any transepidermal migration).
The INI-1 immunostain shows loss of expression. (Endothelial cells act as internal control).
Out of these differential diagnoses, epithelioid sarcoma, epithelioid MPNST and myoepithelial carcinomas are known to show loss of INI-1 expression (deletion of SMARCB1 gene).
The immunoprofile (positive for CK, calponin, S-100 and p63) also favours a myoepithelial phenotype.
Thus, the most appropriate diagnosis is myoepithelial carcinoma (with atypia and mitosis).
Amyloidosis, thick sections
Biopsy shows a nodular collection of acellular, pale eosinophilic, fibrillary material in the dermis, suspicious of amyloidosis. Congo red (CR) staining with polarizing microscopy is required for confirmation of the diagnosis. Once the diagnosis is confirmed, various immunohistochemictry/ mass spectrometry/ proteomic studies may be conducted to determine the nature of the amyloid in the tissue.
The thickness of the section is critical for Congo Red staining. While the thickness of the section for routine histology varies from 2-5 micron, depending on the organ, the section for Congo Red staining needs to be thicker. One needs to instruct the histo-technician to cut an 8-10 micron thick section. This is especially required when the amount of amyloid is scanty. Increased thickness of the section allows the light to pass through multiple planes, allowing an effective birefringence.
Dermatophytosis, necrobiosis lipoidica
Sandwich sign finds more than one mention in dermatopathology.
Sandwich sign is found in dermatophytosis. In early dermatophytosis, the fungal hyphae are sandwiched between two layers of stratum corneum. The upper layer shows normal compact orthokeratosis. The lower layer is abnormal, composed of a combination of orthokeratotic and parakeratotic cornified layers. This is known as the sandwich sign, which was initially described by Dr Bernard Ackerman. This is an important clue for early dermatophyte infection.
Another condition where sandwich sign is described is necrobiosis lipoidica. Here necrobiosis is usually discontinuous and shows alternate layers of necrobiotic collagen and inflammatory cells, in between normal collagen bundles.
ALK positive anaplastic large cell lymphoma
The biopsy shows diffuse infiltration of the dermis by atypical lymphoid cells. The cells are positive for CD45, CD30 and ALK1, while negative for other B cell, T cell and myeloid markers. Thus, this is a case of anaplastic large cell lymphoma (ALCL). ALCL is classified based on ALK expression/ rearrangement into two groups: ALK positive ALCL and ALK negative ALCL. As this case expresses ALK1 by immunohistochemistry, the correct diagnosis is ALK positive ALCL (only mentioning ALCL is not considered correct).
Primary cutaneous ALCL are predominantly ALK negative. Very few cases of ALK positive primary cutaneous ALCL have been reported in the literature. Most cases of cutaneous ALK positive ALCL are a spectrum of systemic ALK positive ALCL with secondary cutaneous involvement. These patients should be investigated for systemic ALCL. As this patient had regional lymph node enlargement, he should be further investigated for lymphadenopathy in other body regions by imaging (MRI/ PET scan), FNAC/biopsy from lymph node for lymph node involvement by lymphoma (for primary cutaneous vs systemic lymphoma) and bone marrow biopsy for staging.
Atypical pANCA pattern on ANCA spot test
This is an indirect immunofluorescence test, called ANCA spot that uses an ethanol-fixed smear of neutrophils. The common patterns of staining include cytoplasmic granular staining (cANCA) and peri-nuclear staining with nuclear extension (pANCA).
In this case, there is strong peri-nuclear staining without nuclear extension. This is known as atypical pANCA pattern. The two main target antigens of ANCA-associated vasculitis are myeloperoxidase (MPO) and proteinase 3, however, many minor antigens also exist, antibodies against which can give atypical staining patterns.Atypical pANCA pattern of staining can be seen in other diseases as well such as SLE, inflammatory bowel disease etc.
Usually, ANCA spots are used as a screening test. It should be confirmed by some other method. The commonly used confirmatory methods include immunosorbent techniques, such as ELISA, immunoblot or line blot.
Indirect immunofluorescence (IIF) on rat bladder mucosa
is the confirmatory test to diagnoses paraneoplastic pemphigus. These patients often have serum antibodies against the plakin family of proteins. Plakin antigens are present in the urinary bladder mucosa. Thus, IIF against rat bladder mucosa can detect intracellular patterns of immunoglobulin deposition.
The sample required is the patient's serum.
Other methods to detect anti-plakin antibodies are immunoprecipitation, ELISA, antigen mapping etc. with lower sensitivity.
Direct immunofluorescence (DIF) in cases of PNP shows immuno-deposits in the intercellular junction and basement membrane zone. However, this pattern is not seen in all cases and may not be specific.
Cookie cutters; a sign seen in scleroderma/morphea is named after them
On scanning magnification, the histological features of morphea include cookie cutter sign, square biopsy sign and high eccrine glands. Cookie cutter sign is defined as presence of straight and parallel lateral edges of the punch biopsy specimen, such as that made by a cookie cutter in cookie dough. Square biopsy sign is defined as a biopsy in which the 4 corners of the tissue sections each form approximately 90 degree angles, that is, a rectangle or square. These features are found in 70-90% biopsies of morphea.
Fluorescein isothiocyanate (FITC)
FITC is the most commonly used flurochrome in routine practice.
Flurochrome is a chemical substance, which is when excited with a light of a particular wavelength, it goes into a higher energy state. Then while returning to its basal energy state, it emits light of higher wavelength. This difference of wavelength can be detected using a UV microscope. FITC has excitation and emission spectrum peak wavelengths of approximately 495 nm/519 nm, giving it a green color.
The false statement is c. It is an indolent tumor, and behaves less aggressively compared to melanoma.
All other options were correct.
Markel cell carcinoma (MCC) is the prototype of primary neuroendocrine carcinoma of the skin. It is derived from Markel cells of the skin. With immune deficiency, there is increased incidence of MCC and most of these tumors are linked to MC polyoma virus (MCPyV).
Histologically MCC shows sheets, nests, trabecular or a mixed pattern. The tumor cells show small blue round cell morphology. They exhibit high mitosis and apoptosis. On immunohistochemistry, MCC cells express neuroendocrine markers (synaptophysin, NSE, chromogranin, CD56), pan cytokeratin and CK20. CK20 is consistently expressed by MCC. In fact, CK20 is used to differentiate MCC from other neuroendocrine carcinomas.
MCC can arise within other adnexal tumors, can show melanocytic differentiation and BCC like differentiation with presence of nested growth pattern, mucinous stroma and cleft formation.
MCC shows an aggressive behaviour (much aggressive compared to melanoma). It shows rapid progression, frequent local recurrence and local lymph node metastasis.
The slide shows several artefacts.
The most prominent artefact is that alternate sections are damaged and lightly stained. This is called alternate thick and thin sections. This occurs most commonly due to loose blade or block in the microtome.
Another artefact seen here is parallel vertical lines in the epidermis, which is known as the chatter artefact. This occurs due to vibrations of knife edge or excessive steep clearance angle or different consistency of different tissues in the block.
This is not a punch/ squeeze artefact as it is not seen in all the sections. An artefact during processing will similarly produce the changes in all serial sections, which is not present here.
Joseph von Gerlach
He was an eminent German anatomist and pioneer of histology. He devised various techniques to assess the fine structure of tissues, most notably a procedure of staining histologic sections that marked the beginning of routine staining in histology. Gerlach was also one of the pioneers of microphotography.
Reference: Weyers W. Joseph von Gerlach-A Reminder of One of the Pioneers of Histochemistry on the Occasion of His 200th Birthday. Am J Dermatopathol. 2020;42:731-38.
This is a transmission electron microscopy (TEM) section of skin biopsy. The stain used is double staining by uranyl acetate and lead citrate.
The biopsy shows a small split at the dermoepidermal junction at the sublamina densa level. With the clinical findings, this is diagnostic of epidermolysis bullosa dystrophica (dystrophic EB).
EB is a rare form of genodermatosis. TEM is considered as one of the most important diagnostic modality of EB, along with antigen mapping and molecular diagnostic techniques. TEM is very useful in identifying the level of split.
For further detail about role of TEM in EB, you can refer to the following article:
Eady RA, Dopping-Hepenstal PJ. Transmission electron microscopy for the diagnosis of epidermolysis bullosa. Dermatol Clin. 2010;28:211-22
Indeterminate dendritic cell tumor (IDCT), also known as indeterminate cell histiocytosis
Electron microscopy shows presence of abundant lysosomes, endosomes and membrane bound dense granules within the cytoplasm of these atypical histiocytoid cells. These cells show nuclear irregularity and infolding of nuclear membrane. They lack Birbeck granules, characteristic of Langerhans cell histiocytosis (LCH). [Only ‘absence of Birbeck granules’ is not considered a correct answer]
IDCT is a rare histiocytic lesion that has morphological similarity with LCH. Clinically IDCT presents as nodular lesions in adults. Histology shows atypical histiocytoid cells in the dermis, with variable accompanying inflammatory cells. Eosinophilic infiltrate is not a prominent feature. On immunohistochemistry, the tumor cells show immunoprofile similar to LCH, i.e; they express CD1a, S100 and CD68 (variable), but in contrast to LCH, they don’t express Langerin (CD207). The outcome is usually favourable.
EBV-associated mucocutaneous ulcer
EBER in situ hybridization should be performed to confirm the diagnosis.
Epstein-Barr virus (EBV
positive mucocutaneous ulcers (EBVMCUs) were first described as a lymphoproliferative disorder in 2010. Clinically, EBVMCUs are shallow, sharply circumscribed, unifocal mucosal or cutaneous ulcers that occur in immunosuppressed patients. In general, patients exhibit indolent disease progression and spontaneous regression.
Histologically, EBVMCUs are characterized by the proliferation of EBV-positive, variable-sized, atypical B-cells. The localized mucosal or cutaneous ulcers are characterized by the presence of EBV-positive atypical immunoblasts or Reed Sternberg-like cells, accompanied by dense polymorphic infiltration with the variable presence of other inflammatory cells. The atypical cells express CD30, with variable expression of CD15 and B cell markers (CD20, PAX5, BOB1).
PRKAR1A
The condition mentioned here is pigmented epithelioid melanocytoma (PEM).
PEM are small to large (4-30 mm) pigmented papules commonly located on the head and neck or lower extremities occurring at a mean age of 20 years in both genders.
Histologically, PEM are wedge-shaped, intradermal lesions composed of large, pigmented epithelioid, spindled, and dendritic melanocytes and abundant heavily pigmented melanophages.
PEM is an intermediate grade melanocytic lesion with a rate of lymph node involvement of approximately 40-46% however, extranodal and distant metastases are extremely rare. The commonest genetic alteration is loss of heterozygosity of PRKAR1A (protein kinase A regulatory subunit 1 alpha) locus.
The most likely diagnosis is NUT midline carcinoma.
IHC to confirm the diagnosis is NUT (nuclear protein in testis).
NUT midline carcinoma is a rare, genetically defined, aggressive tumor. This is genetically defined by rearrangement of NUT gene located on chromosome 15q14. It affects midline structures. Histologically it shows undifferentiated high grade tumor with abrupt squamoid differentiation and keratin pearl formation. Positivity for NUT immunohistochemistry is diagnostic of this condition.
Other differential diagnosis that can be considered in such situation are poorly differentiated squamous cell carcinoma and small cell carcinoma. However, p40 is a highly sensitive marker for squamous cell carcinoma. If it is negative, SCC is highly unlikely. Squamous differentiation can be seen in neuroendocrine tumors, but extremely uncommon in small cell carcinoma. Considering the location and the presentation, NUT midline carcinoma is the most suitable diagnosis in this case.
The correct answer is D
This is a case of cutaneous gouty panniculitis.
It contains monosodium urate crystals in dermis and subcutaneous fat producing panniculitis. It is a manifestation of chronic gout. However, urate crystals are water soluble and get dissolved in routine formalin-based processing. Thus, on routine histological processing, we can’t see the urate crystals. Gouty panniculitis appears as fibrillary pale eosinophilic material, surrounded by lymphocytes, macrophages and giant cells. This pale fibrillary material represents the dissolved urate crystals. The negatively birefringent urate crystals can be demonstrated either in fluid preparation (by FNAC) or by alcohol processing of the biopsy material (instead of formalin processing).
1. Histology of cutaneous nodule would show leiomyoma.
2. Immunostain used in figure D is fumarate hydratase (FH), which is lost in tumor cells. Endothelial cells act as positive control (cytoplasmic staining)
The patient here is likely to have hereditary leiomyomatosis and renal cell carcinoma (HLRCC) syndrome. She presented with multiple cutaneous leiomyomata and renal tumor. The histology of renal tumor shows papillary and solid areas with cells showing prominent nucleoli. This type of histology is very characteristic of HLRCC. The tumor shows loss of fumarate hydratase (FH) expression. There is a germline mutation of the FH gene. HLRCC associated renal tumors most often belong to this fumarate hydratase deficient renal cell carcinoma. The most common histological differential diagnosis is type 2 papillary renal cell carcinoma. These patients often present with early onset cutaneous and uterine leiomyomas and subsequently develop FH deficient RCC. Thus, germline FH gene testing is important for screening of these patients.
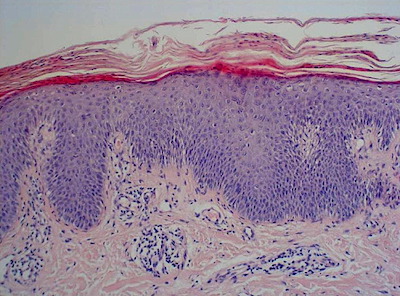
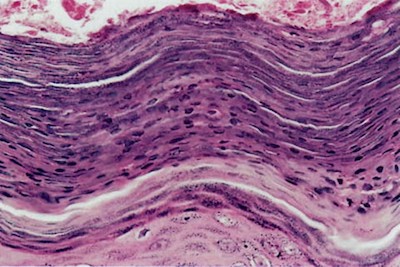
Bowen's disease
The answer is windblown appearance and eyeliner sign seen in Bowen’s disease.
In Bowen’s disease (squamous cell carcinoma in situ), there is full thickness dysplasia of the epidermis. There is complete loss of polarity of the keratinocytes (windblown appearance), but the basement membrane remains intact and the basal keratinocytes are usually spared (eyeliner sign).
